Updated 2:25 p.m., July 23
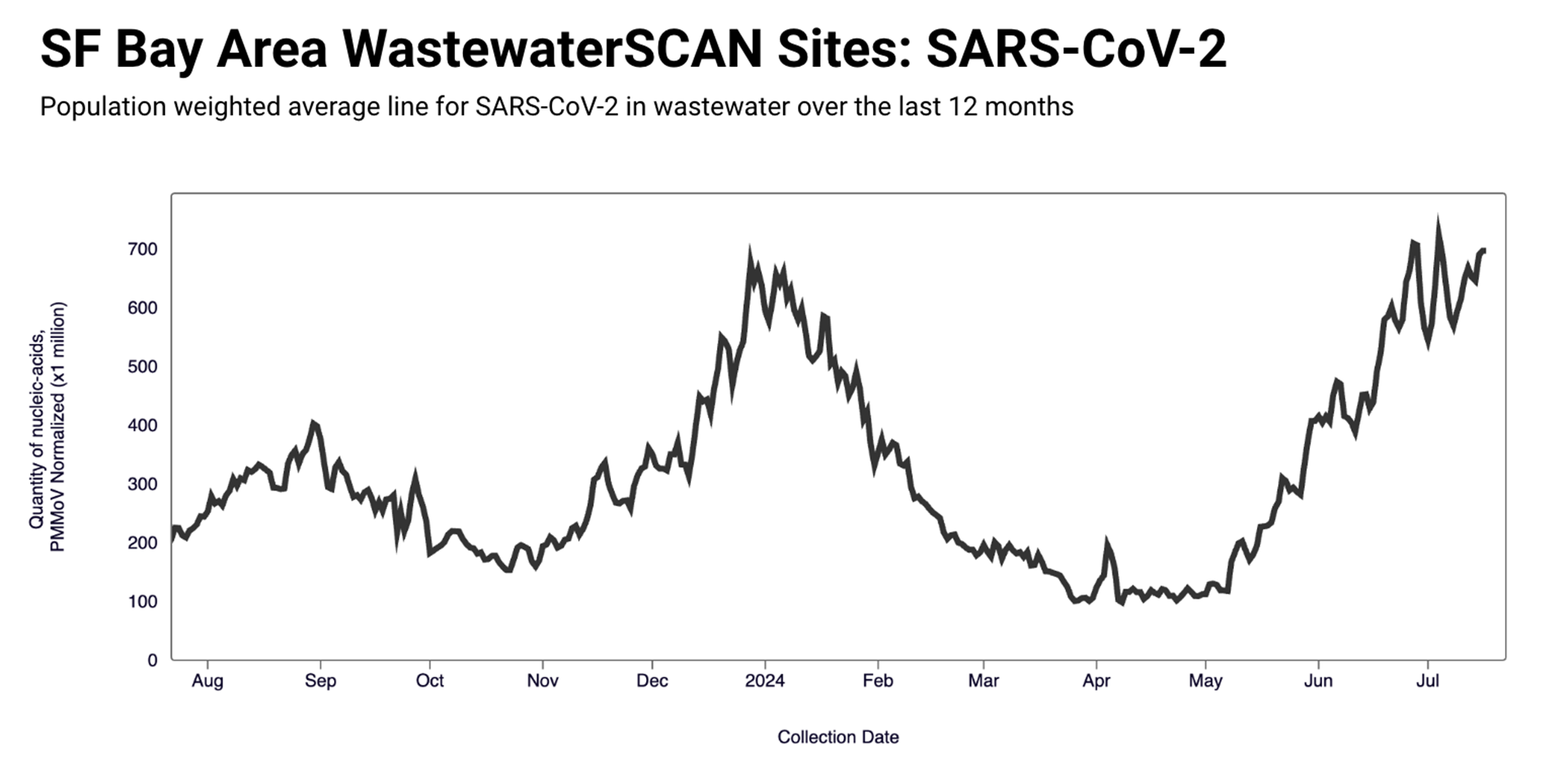
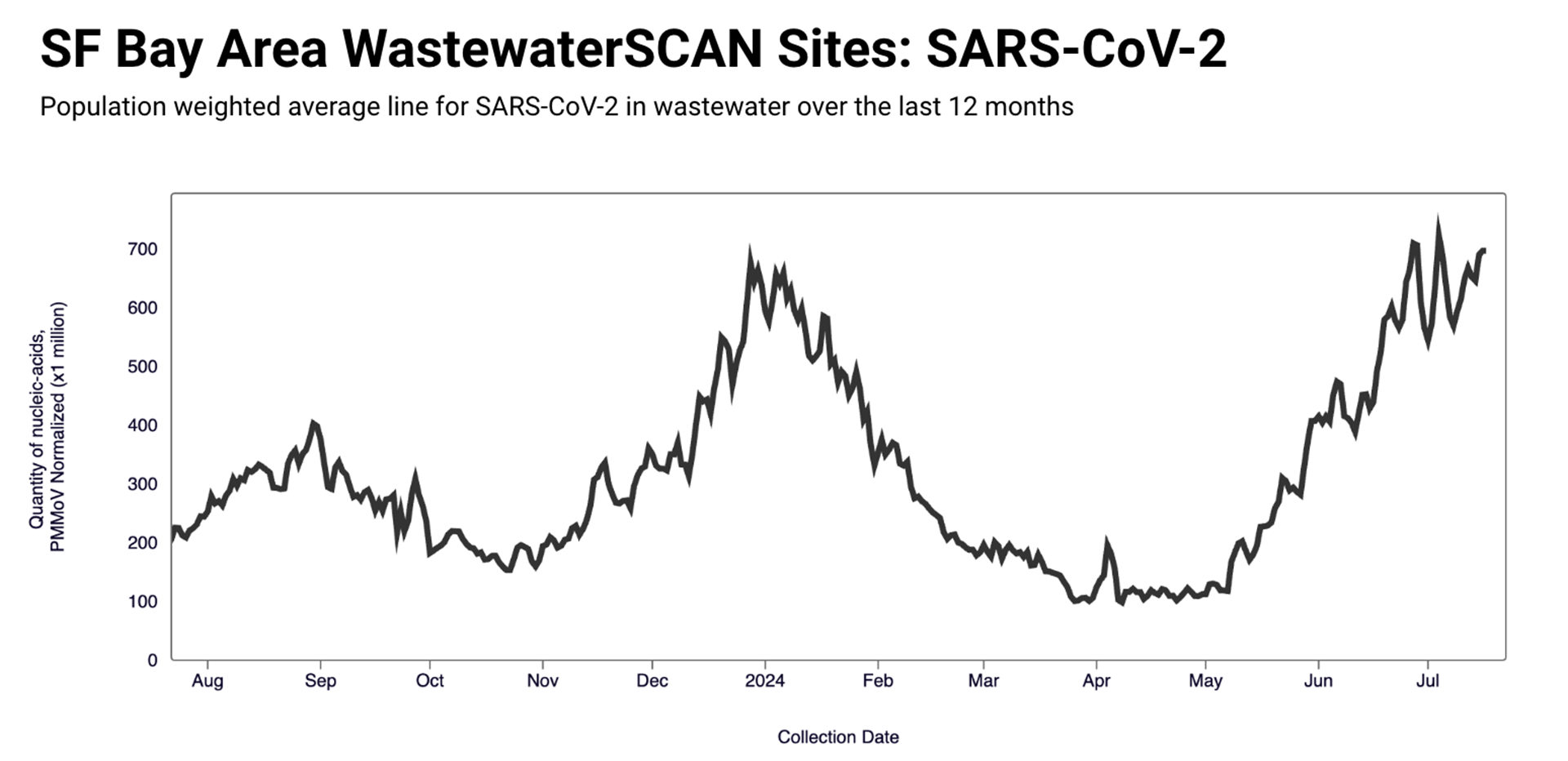
Levels of COVID-19 in the Bay Area’s wastewater are continuing to rise — and now, those numbers are as high as they were during the last winter surge of infections.
Data from Stanford University’s WastewaterSCAN project, which monitors the presence of COVID-19 and other viruses in human sewage across the U.S., indicates that COVID-19 levels are still on the rise across 61% of the sites monitored around the Bay Area. Statewide, California is currently in the “Very High” category for levels of the virus in wastewater, according to the Centers for Disease Control and Prevention (CDC.)
WastewaterSCAN’s Amanda Bidwell told KQED by email that COVID-19 has been detected in 100% of Bay Area sewage samples they’ve collected over the last three weeks. (If you have COVID-19, the virus will show up in your feces soon after you’re infected.)
Keep reading for what to know about this rise in Bay Area COVID-19 levels, or jump straight to:
- What’s the current COVID contagion and isolation guidance?
- How much are new COVID variants driving this rise?
- Are there any new 2024 COVID symptoms?
- Who is the most at risk for COVID right now?
What’s going on with COVID in the Bay Area’s wastewater right now?
The Bay Area’s own COVID-19 wastewater levels are “higher than where they were this time last year and on average as high as we saw during the winter peak earlier this year,” said WastewaterSCAN’s Bidwell.
In the last weeks, the Stanford team has observed a particularly pronounced rise in San Francisco’s wastewater. Bidwell told KQED that the data shows “some of the highest wastewater levels we’ve observed at these 2 SF sites to date.”
The San Francisco Department of Public Health told KQED in a June 11 email that it’s “difficult to determine an exact cause of why COVID-19 detections have increased” locally, noting that “it can be the result of various factors, including waning immunity, the increase in travel and gatherings associated with the summer season, and the emergence of new subvariants.”
The agency also pointed to the seasonal behavior of the virus in previous years, notably the “increase in COVID-19 activity around late spring to late summer, followed by another increase during the winter.”
Nationally, COVID-19 wastewater levels have kept rising across the country, and levels of the virus are currently classified as “High” on WastewaterSCAN’s dashboard of all its sites around the United States.
You can check the COVID-19 levels in your own county’s wastewater according to WastewaterSCAN’s monitoring:
San Francisco | Alameda | San Mateo | Santa Clara | Contra Costa | Solano | Marin | Sonoma | Napa
- Jump straight to: How should I be altering my behavior during a rise in COVID?
COVID swelled earlier this summer than it did in 2023. Why?
In 2023, “late June is when we started to see a summer increase,” said WastewaterSCAN’s Bidwell — but this 2024 swell started several weeks earlier than that.
It’s undoubtedly become harder in 2024 to materially track COVID-19 levels in a certain area. As of May 1, the CDC no longer requires hospitals nationwide to report the number of patients admitted with COVID-19. This had been one of the remaining indicators of rising COVID-19 levels in an area, along with PCR tests. Now, health officials must rely on a combination of wastewater data and hospital deaths of patients with COVID-19.
According to the California Department of Public Health (CDPH), the state’s seven-day test positivity rate — the average percentage of people each week who get a positive diagnostic test result from a lab after taking a PCR test — has kept rising since April 27 (from 1.9% to 12.8%, with the last available data from July 15).
However, since this data doesn’t include at-home antigen testing, it doesn’t represent the full picture of COVID-19 positivity around the state.

“Of course, it’s hard to use wastewater to tell you how many people that represents,” said Dr. Peter Chin-Hong, an infectious disease expert at the University of California, San Francisco (UCSF), of the recent observed rise in sewage. “But nevertheless, the trend is important.”
As for why the Bay Area could now be seeing a summer rise in COVID-19 wastewater levels over a month earlier than it did in 2023, Chin-Hong said a big factor is our collective waning immunity against the virus.
“One year ago, last year, many more people had gotten additional vaccines,” he said. “They had additional immunity that was more recent.”
But in 2024, “we only have about 22% or so of Americans vaccinated” nationally, Chin-Hong said. In California, only 14.9% of people statewide are up-to-date on their COVID-19 vaccines. So if someone hasn’t been infected with COVID-19 recently and they haven’t gotten the latest vaccine, they’re left extra-vulnerable to rising COVID-19 levels in their community.
How much are new COVID variants driving this rise?
You might hear about new COVID-19 variants informally called “FLiRT”: KP.1.1, KP.2 and KP.3.
These latest omicron descendants, nicknamed for the letters used for their mutations, have risen in prominence recently around the country, overtaking the previous leading variant, JN.1 — the one that “was ruling the roost for a lot of the winter and spring,” Chin-Hong said. Now, KP.3 has become the most dominant strain nationwide.
In the Bay Area, WastewaterSCAN’s Bidwell said that KP.2 is still the dominant variant in the three Bay Area wastewater sites where the Stanford team sequenced this data on specific variants.
The new variants matter because each new one brought increased transmissibility during the pandemic. This means that although much of the general population will not get particularly sick with these new COVID-19 variants when they become dominant, there will still be higher-risk groups that will get seriously ill, Chin-Hong said.
“Maybe that’s the fact of life, but my point is: It shouldn’t be the fact of life because we have so many tools” to reduce COVID-19 spread and treat infectious people, Chin-Hong said.
The CDC has also stated that based on current data, “there are no indicators that KP.2 would cause more severe illness than other strains.”
As for the reformulated seasonal COVID-19 vaccine, the Food and Drug Administration (FDA) recommended on June 5 that the new, updated COVID-19 vaccine that will be offered in the fall should in fact be based on the JN.1 variant.



