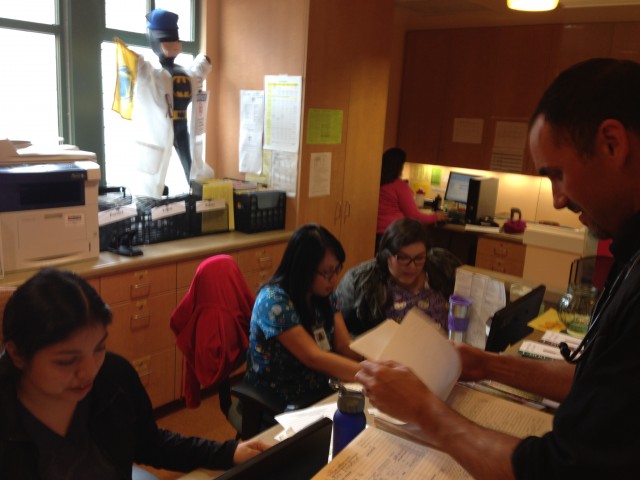
Clinic medical director Dr. Davi Pakter says the long wait is one side effect of adding nearly three million people to Medi-Cal since January, 2014. At his clinic, the patients with the greatest need are seen first.
“We try very hard to arrange our schedules so that we can accommodate folks that are in urgent need," he said, "and try to avoid sending folks to the emergency room -- which is a much higher cost and usually not in the best interest of the patient.”
Pakter says that means people who need a check-up or treatment for a less urgent condition can end up waiting one to two months.
A lot of Medi-Cal patients are turning to federally subsidized clinics like LifeLong because private practice doctors won’t accept Medi-Cal insurance.
“They’re not able to afford it,” says Dr. Del Morris, the president of the California Academy of Family Physicians. Morris says the state’s notoriously low reimbursement rate -- one of the lowest in the nation -- won’t cover the cost of caring for Medi-Cal patients.
“These patients, because of their social circumstance have a higher acuity level than an average patient of the same age,” he says. “These are complicated patients with complex problems and take up a lot of a physician’s time. To be taking on patients like this and lose money in the process is just not something most private practices are willing to do.”
Morris who’s also the medical director of the Stanislaus County Health Services Agency -- says Medi-Cal patients are often forced to get care at emergency rooms.
Morris expects the situation to worsen, unless state lawmakers take action.
A provision of the Affordable Care Act that temporarily boosted Medi-Cal reimbursement rates expired on December 31. Also, state lawmakers passed a ten percent cut to California’s reimbursement rates during the depths of the state’s recession took effect last month for primary care doctors.
State lawmakers Sen. Ed Hernandez (D-La Puente) and Asm. Rob Bonta (D-Alameda) introduced a bill this week that would restore the higher reimbursement rates. But even if it passes, they’ll have to persuade Gov. Jerry Brown to sign it.
H.D. Palmer with the state’s finance department says the governor’s not budgeting for higher provider rates because California faces numerous fiscal uncertainties.
“So we have to be very careful and prudent about adopting any new major spending commitments or dealing with some of the difficult but necessary reductions that had to be made in recent years,” he said.
California’s spending on Medi-Cal will jump by $1.7 billion in a just a few years. Right now and through 2016, the federal government pays 100 percent of the cost of covering people who are eligible under the Medicaid expansion. From 2016 to 2020, the contribution will gradually decline to 90 percent, meaning California must pick up the rest.