On the education front, Pre-Health Dreamers, a network of hundreds of health career-bound undocumented students, estimates nearly 70 DACA recipients are enrolled in medical schools across the country, while hundreds more are studying allied health fields.
California as a whole faces a shortage of thousands of primary care providers as soon as 2025, according to a report released this month by Spetz and other researchers at UCSF. Most hospitals in California are already having difficulties recruiting experienced nurses, particularly in emergency rooms and intensive care units, said Spetz.
“There is a real need for experienced nurses now, both because hospitals need to have nurses with experience to carry out the more complicated tasks, and also to help mentor and prepare new graduates that are coming into workforce,” said Spetz.
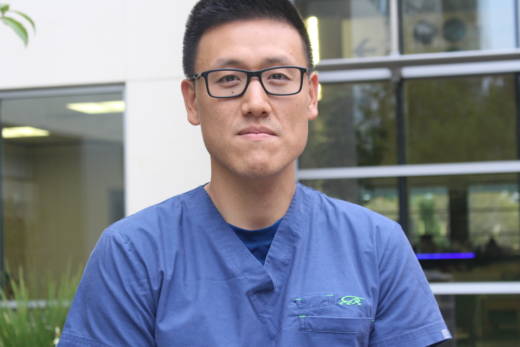
That makes DACA recipients like Eli Oh a hot commodity. He’s a nurse who is part of a roving emergency response team at Stanford Health Care. Oh also works a second job as a traveling intensive care nurse at San Jose’s Regional Medical Center and other hospitals in the South Bay.
“If you’re someone who doesn’t handle stress well this might not be the job for you because someone is dying in front of you, and you’re responsible,” said Oh, after just finishing his graveyard shift one recent morning.
Staying calm while helping patients come back from the brink of death in the middle of the night might seem like a grueling schedule to plenty of people, but Oh said it’s not as tough as what he’s been through already.
Oh was 11-years-old when he came from South Korea with his family. They arrived on a tourist visa, escaping the Asian financial crisis of the 1990s, and stayed. His dad had lost his job as an industrial engineer in Korea, and was not proficient in English. He could only find work as a house painter in the U.S., Oh said.
“There were a lot of winters where we just couldn’t make rent,” said Oh, who grew up in the Cupertino area. “I grew up getting evicted.”
When he was 21, and working as a waiter to pay his way through nursing school, his family got evicted once more. Oh had to pick up another under-the-table job to keep a roof over his family’s head, he said.
“I was going to nursing school full time and pulling 16-hour days That was probably the hardest time of my life. I was paying rent for my entire family for months,” he said.
One thing that kept Oh going was the hope that, one day, he could work legally as a nurse. He had done his research, and knew that nursing skills were in increasing demand and well compensated.
When President Obama used executive action to create DACA in 2012, Oh signed up. He has been able to work as a nurse for five years, and he was initially saddened by the news that the Trump administration was ending the DACA program. But Oh also feels grateful for the chance he had to gain professional experience.
“DACA has given us so many of us the skills, the resources and the education that we need to survive as immigrants anywhere in the world,” said Oh, 30. “And so I could be angry and bitter, you know a lot of us struggle with that. But I’m choosing gratitude instead.”
Oh’s employers at Stanford Health Care declined to comment for this story, but pointed us to a letter sent by Stanford University President, Marc Tessier-Lavigne, to the White House.
Investing in the education of DACA holders, “is an investment in our country’s future, as they apply their talents to strengthening our society and to driving economic growth,” wrote Tessier-Lavigne.
Stanford Health Care’s jobs website currently shows more than 110 openings in nursing, including 11 positions for critical care nurses in intensive care, neurosurgery and other teams in Palo Alto.
Across the San Francisco Bay, a nonprofit health center, La Clinica de la Raza, has 12 job openings at its network of community clinics in Solano, Contra Costa and Alameda counties.
If DACA ends, La Clinica could lose about 10 percent of its employees as their work permits expire, said Jane Garcia. These are staff members who might be working as social workers, receptionists, medical assistants, therapists, dental hygienists and in other fields.
“The whole possibility that I would lose a big chunk of my workforce that is bilingual, that lives in the community, is daunting, extremely sad and problematic,” said Garcia, whose clinics see more than 90,000 patients per year, especially in the Bay Area’s large immigrant communities. “It’s very costly to recruit and hire regular staff and so it’d be very, very disruptive to our operations.”
Employers like Stanford and La Clinica could spend about $20,000 to recruit and train replacements for registered nurses and even more for specialized nurses, said Spetz, the UCSF researcher.
But for the nurses themselves, there is no shortage of work opportunities in other countries, she said.
“Nurses who might get pushed out of their jobs in the U.S. will easily be able to find work in Canada, Australia, England, Ireland and developing countries,” said Spetz.
Moving to Canada is a possibility that Oh, the critical care nurse, is keeping in mind if he becomes unable to legally work in the U.S. But he would prefer to stay and work in the San Jose area, where his family lives.